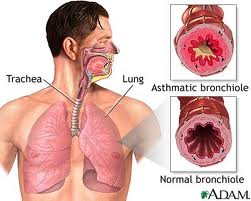
Guiding Patients Through Decisions in Idiopathic Pulmonary Fibrosis (IPF): The Respiratory Therapists' Role- Idiopathic pulmonary fibrosis (IPF) is a rare, progressive lung disease that greatly impacts patients' quailty of life and diminishes life expectancy. New therapies are available that slow function decline. These therapies are used in combination with oxygen supplementation, pulmonary rehabilitation, symptomatic treatment, and supportive care. This program will discuss the prevalence, signs and symptoms, and diagnostic criteria for IPF as well as compare and contrast available therapies and formulate strategies for comprehensive management of symptoms.
Outline the prevalence, signs and symptoms, and diagnostic criteria for IPF.
Compare and contrast available therapies for IPF.
Formulate strategies for comprehensive management of symptoms.
Effectively counsel IPF patients on available therapies and supportive care.
Identify patients with IPF who may benefit from intensification of therapy.
Guiding Patients Through Decisions in Idiopathic Pulmonary Fibrosis (IPF): The Respiratory Therapists' Role- Idiopathic pulmonary fibrosis (IPF) is a rare, progressive lung disease that greatly impacts patients' quailty of life and diminishes life expectancy. New therapies are available that slow function decline. These therapies are used in combination with oxygen supplementation, pulmonary rehabilitation, symptomatic treatment, and supportive care. This program will discuss the prevalence, signs and symptoms, and diagnostic criteria for IPF as well as compare and contrast available therapies and formulate strategies for comprehensive management of symptoms.
Outline the prevalence, signs and symptoms, and diagnostic criteria for IPF.
Compare and contrast available therapies for IPF.
Formulate strategies for comprehensive management of symptoms.
Effectively counsel IPF patients on available therapies and supportive care.
Identify patients with IPF who may benefit from intensification of therapy.1.0 Free CEUs for Respiratory Therapists
Expires 12/31/17